The threat of AMR for people living with HIV: A South African doctor’s perspective
Two graphs, two lines. On the first, a steady downward slope. On the second, a steep drop, and then a gently downward trend. The first line represents the estimated number of people newly infected with HIV in South Africa, down 57% since 2010. The second line represents the estimated number of deaths due to AIDS in South Africa, down 70% since 2010.
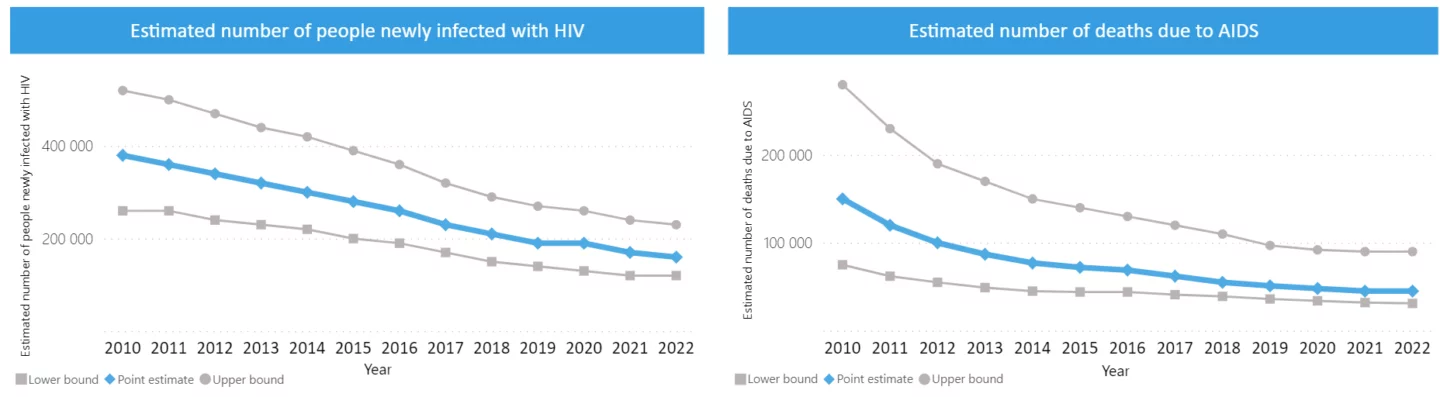
Source: https://cfs.hivci.org/index.html
In South Africa, there is progress against this deadly disease, driven in large part by free access to antiretroviral medications, starting in the early 2000s for certain population groups and, since 2016, for all people living with HIV in South Africa.
But future progress is in jeopardy.
“Antimicrobial resistance is one of the absolute top things that could set back progress in HIV patients. I mean we have the HIV drugs now—that’s not the limiting factor. One of the things that might make things go backwards is AMR,” says Dr Jeremy Nel.
Jeremy would know. As the Head of Infectious Diseases at the Helen Joseph Hospital in Johannesburg, South Africa—one of the biggest hospitals in Johannesburg and one of the biggest HIV clinics in the world—he treats patients with HIV, tuberculosis, and other communicable diseases every day.
Antimicrobial resistance (AMR) can affect people living with HIV/AIDS in two ways. AIDS is caused by the human immunodeficiency virus (HIV), which may develop resistance toward antiretroviral medication in a patient, especially if that patient does not take medication regularly. HIV drug resistance—as this particular type of antimicrobial resistance is called—can develop within a patient, and it may be passed between infected sexually active people or from mother to newborn child.
But people living with HIV/AIDS are also particularly vulnerable when it comes to bacterial AMR. They carry significantly higher risks for serious bacterial infections, one of the most common causes of death of people living with HIV worldwide.
HIV-positive people frequent hospitals more, where they are more likely to pick up serious bacterial infections. Their immune systems are weaker, making serious bacterial infections more common. And if they are treated with antibiotics, their antiretroviral medication may diminish the efficacy of that treatment, thus opening the door for resistance to develop.
‘‘AMR has always been an issue, but it’s getting more acute. Resistance toward antibiotics and antifungal agents—whether for use in HIV patients or not—has become palpably worse. We are starting to see patients with infections in the hospital where I work for which there is just no effective treatment, and that wasn’t the case five years ago,” says Jeremy.
“One of the great challenges with all antimicrobial resistance is it’s always additive. You almost never go backwards. You can at most stabilize and slow things down, but you almost never get an antibiotic back, so to speak. So it’s kind of this relentless march, and we just have fewer and fewer antibiotics left,” says Jeremy.
