Gonorrhoea: The past, present and future of an ancient disease
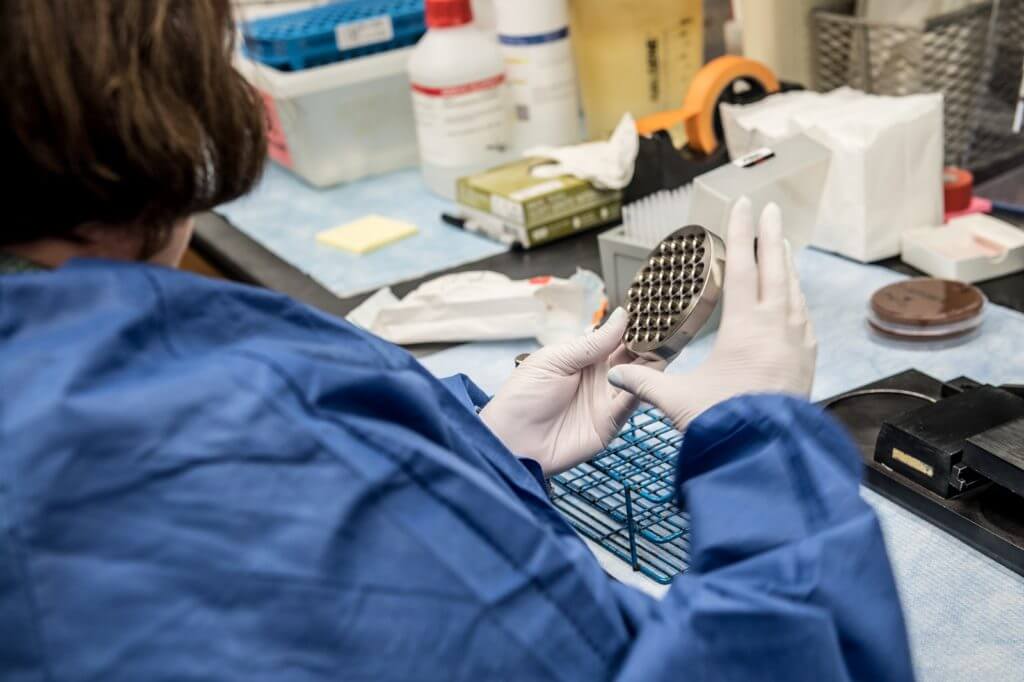
Paula Dixon, Lab Manager at the Division of Infectious Diseases at the University of Alabama at Birmingham, prepares a culture of gonorrhoea for testing. Dixon’s lab serves as a repository for all sites involved in GARDP’s zoliflodacin trial.
Gonorrhoea is an infection caused by the Neisseria gonorrhoeae bacterium. It spreads through vaginal, anal and oral sex and can infect the penis, vagina, rectum and throat. The infection is ancient, with the first known description – in Chinese medical textbooks – dating back to 2600 BC.
Throughout the centuries, a range of “treatments” have been used for gonorrhoea. Among the earliest was mercury, with silver nitrate, arsenic, bismuth and even gold recommended at different times. These metals were administered as irrigations or injections into the urethra.
Ingredients derived from animals and minerals were also used to treat the symptoms of gonorrhoea. Pierre Pomet in his Compleat History of Druggs, published in 1712, noted that powdered coral is “cooling, drying and binding … and is profitable in Gonorrhoea.” Pomet also recommended the powdered tips of sea crab’s claws.
One of the more spurious remedies for gonorrhoea involved clapping both sides of the penis with hard objects in an attempt to push the discharge from the urethra, while another popular 19th century “cure” involved the use of cubebs, an Indonesian pepper which was dried and powdered, and balsam of copaiba, which was extracted from a South American tree.
A discovery that changed everything
Then, in 1879, the German physician Albert Neisser discovered the bacterium responsible for gonorrhoea, which transformed our knowledge of the infection and paved the way for truly effective antibacterial treatments.
Sulfonamide drugs (commonly called sulfa drugs), introduced in the 1930s, were the first broadly effective antibacterials used to treat gonorrhoea. However, by 1944 resistance had emerged and treatment failure rates exceeded 30% in people treated with maximum sulfonamide doses.
The availability of penicillin in the 1940s revolutionized treatment of bacterial infections and quickly become the preferred gonorrhoea drug.
The rise of drug-resistant gonorrhoea
However, soon after the first penicillin-based antibiotics were introduced, resistance became apparent as increasingly larger doses were required. During the 1970s, resistance to tetracycline (another drug used to treat gonorrhoea) also emerged. By 1986, the World Health Organization (WHO) recommended penicillins and tetracyclines only be used with gonorrhoea in areas of the world where antimicrobial resistance was low. Eventually they were abandoned altogether.
Over time, gonorrhoea has proven itself capable of slipping past antibiotics and acquiring resistance to an increasing number of once reliable drugs. In a recent WHO survey of 77 countries, 97% noted resistance to commonly used gonorrhoea treatments and 66% reported at least one case of resistance to cephalosporins, the last option for treatment with a single drug.
A new gonorrhoea treatment
Neisseria gonorrhoeae is now identified by the WHO as a priority infection urgently requiring new antibiotics. To address the lack of effective drugs, the Global Antibiotic Research and Development Partnership (GARDP) is developing a new treatment for gonorrhoea and is working to ensure it is available to everyone who needs it, wherever they live.

Dr Jodie Dionne-Odom, Chief of Women’s Health Services at 1917 HIV Clinic of the University of Alabama at Birmingham, prepares to see a patient. Dr Dionne-Odom is a Site Principle Investigator for the GARDP zoliflodacin trial.
GARDP is partnering with biotech Entasis Therapeutics on a novel antibiotic called zoliflodacin, the only drug being developed specifically to treat gonorrhoea. As a first-in-class treatment, zoliflodacin is active against resistant strains of gonorrhoea. Zoliflodacin has also been designed as an oral treatment option, which has the potential for significant benefits compared to the current standard of care of intramuscular injections.
Following positive phase 2 results, the drug is currently being evaluated in a global phase 3 trial. The trial, which is assessing the effectiveness and safety of zoliflodacin against standard treatments, is expected to enroll 1,000 people with gonorrhoea in the United States, Netherlands, Thailand and South Africa.
Zoliflodacin Trial in South Africa
Three sites across two provinces in South Africa are set to take part in the zoliflodacin phase 3 trial. One is the Wits Reproductive Health and HIV Institute (Wits RHI) which is based at the Hillbrow Health Precinct in Johannesburg, while the other two are South African Medical Research Council (SAMRC) sites in South Africa’s KwaZulu-Natal province. All three sites have wide experience in international trials.
GARDP has partnered with the University of KwaZulu-Natal’s Department of Medical Microbiology for the laboratory aspect of the clinical trial. The work on the trial is expected to enhance the national laboratory STI programme, so that laboratory diagnosis, and not only syndromic management for Neisseria gonorrhoeae, will be available to the broader community and for other clinical trials.